A Different Kind of Disaster Response: Emergency Medical Services and the COVID-19 Pandemic
Jackson D. Déziel
Western Carolina University
Click the Button Below to Download a PDF Version of this Issue Brief
Executive Summary
Emergency medical services (EMS) professionals are largely seen as crisis mediators during acute situations – whether they be traumatic or medical in nature. However, these health care providers (e.g., Emergency Medical Technicians [EMTs] and Paramedics) also serve their communities in a variety of first-response roles. During the ongoing COVID-19 pandemic, their expanded role has been thrust into the spotlight. Training for EMTs and paramedics is multi-faceted and includes Mass-Casualty Incident (MCI) management preparation. Exercises concerning these MCIs, however, typically focus on singular and relatively localized events (e.g., tornado or plane crash). The COVID-19 pandemic has shined a light on the capabilities of EMS professionals and the system as a whole while also exposing areas for improvement. This issue brief explores the role of the EMS professional and how the COVID-19 pandemic has impacted prehospital practice. There exist very real opportunities to bolster the EMS workforce, expand professional roles, and encourage innovation throughout the industry. As we move forward from the COVID-19 pandemic, state-level regulatory and policy change will better prepare us for the next infectious disease event.
1. EMS Providers and Practice
Confusion surrounding EMS professionals and their varying levels of practice is commonplace. All too frequently referred to as “ambulance drivers”, these front-line medical providers can perform advanced assessments and procedures in the emergency setting (although, they are also trained to operate the emergency vehicle). The many levels of EMS professional certainly clouds public perception of the industry, as EMS professionals work in concert with one another to provide the needed emergency care. Training requirements vary by state, but the standard EMS providers levels are Emergency Medical Responder (EMR), Emergency Medical Technician (EMT), Advanced Emergency Medical Technician (AEMT), and Paramedic. [1] Beyond their initial training, paramedics may receive additional certifications in specialty areas, including critical care paramedic, flight paramedic, community paramedic, tactical paramedic, and a myriad of search and rescue disciplines (urban, wilderness, and agricultural).
EMTs and paramedics comprise the largest proportion of EMS professionals, with approximately 27,000 EMTs and 10,000 paramedics in the state of North Carolina. [2] These providers work on ambulances and helicopters/aircraft, and in hospitals and physician offices. The scope of practice for EMS professionals varies across state lines but is driven by the federal Office of EMS within the National Highway Traffic Safety Administration (NHTSA). As the highest level of EMS provider, paramedics are trained to perform advanced invasive procedures (e.g., intravenous access and cricothyrotomy), administer a myriad of medications, and command large-scale incidents (e.g., bus crash). A paramedic’s scope of practice is very similar to that of a Registered Nurse (RN). Paramedics function under physician supervision and employ standing orders, commonly known as “protocols”, which allow them to operate autonomously without a direct physician order for each individual patient. These standing orders inform emergency treatment in the field and allow EMTs and paramedics to function in highly fluid environments. [3]
2. EMS Response to Disasters
EMS professionals are trained to respond to, and manage, complex large-scale events – commonly referred to as Mass-Casualty Incidents (MCIs). These MCI events may present as dramatic as a multi-vehicle collision or as innocuous as a dinner party with collective food poisoning. The defining point, therefore, is the response ability and need for additional external resources. With a renewed focus on MCIs since the COVID-19 pandemic, international researchers in the World Journal of Emergency Surgery established an operational definition of MCIs, finding that they involve multiple victims, disrupt normal functioning, and exceed typical operational capacity. [4]
Specialized MCI training is most often completed through self-study modules offered by the Federal Emergency Management Agency’s (FEMA) Emergency Management Institute and prepares EMS professionals to function within the bounds of the National Incident Management System (NIMS) and its associated Incident Command System (ICS). Through this standardized system, NIMS describes how to work seamlessly with private and public sectors to plan for, respond to, and recover from major incidents. As a supporting framework, ICS guides task-specific responsibilities across responding agencies and jurisdictions during an active event. [5] Additional training can also be completed through FEMA’s Center for Domestic Preparedness (CDP). [6]
Of nearly 3,700 available educational offerings among various federal agencies, 76% of hazard-specific coursework is directly related to chemical, biological, radiological, nuclear, and explosive (CBRNE) response. [7] While biological topics are available, most relate to Ebola and Zika viruses. FEMA inexplicably removed the IS-522 (Exercising Continuity Plans for Pandemics) course in Spring 2020, although IS-520 (Introduction to Continuity of Operations Planning for Pandemic Influenzas) remains available.
The common theme through the vast majority of NIMS and CDP training programs is that of a singular and relatively localized event. EMS professionals who are proficient in NIMS and ICS utilize this management structure to direct resources during events such as bus accidents, carbon monoxide exposures, and various natural disasters. Each of these events has a distinct start/stop point and is relegated to a specific area. Thus, emergency resources can be reallocated from an area that is not experiencing the event to the affected area for a definite amount of time.
This resource management training, however, is rendered inadequate in a situation in which every jurisdiction requires additional resources and there is no estimate for the conclusion of the event. Even in more widespread events, such as hurricanes and tornadoes, there is a distinct sense of when the storm began and ended, and which areas require our focus. With the ongoing COVID-19 pandemic, the timetable is unknown and additional resources are needed everywhere. Recent qualitative research has delved into the views of EMS professionals as they pertain to various large-scale response types. When interviewed, EMS professionals displayed a general level of excitement and thrill towards responses to natural disasters, while they exhibited concern and risk-anxiety for disease outbreaks. [8] How then, do we respond in an environment in which we cannot fully employ our MCI training? Make no mistake: the COVID-19 pandemic is, in fact, a single protracted mass-casualty event.
3. EMS Response to the COVID-19 Pandemic
The SARS-CoV-2 virus and the resulting COVID-19 pandemic have drastically altered the way in which our medical community functions, both emergently and non-emergently. Unprecedented in its scope, the SARS-CoV-2 virus has strained medical resources exponentially more than any other recent pandemic including MERS (2012), the H1N1 Swine Flu (2009), and SARS (2002).[9] As a result, the National Association of EMS Physicians (NAEMSP) has long advocated for a stronger EMS role in disaster management. [10]
EMTs and paramedics have been on the very front-lines of response and initial treatment of COVID-19. As first responders, they are an integral part of the treatment chain. Utilizing a basic response structure developed in the 1960s and 1970s, EMS providers often respond to calls-for-service with little background information. The problem of unbalanced information has been further complicated by the COVID-19 pandemic. Paramedics must now assume that every patient is a possible carrier of the SARS-CoV-2 virus and take the time to don the appropriate protective equipment, increasing response times. [11] The North Carolina Office of EMS (NCOEMS) and the North Carolina College of Emergency Physicians (NCCEP) have developed a High Consequences Pathogens protocol (SC-2) specifically for SARS, MERS, and COVID-19 to guide provider conduct and increase information-sharing while attempting to reduce viral transmission. [12]
During the SARS pandemic of 2002, an analysis of non-SARS EMS calls in a major international city saw demand decrease by 12%.[13] EMS providers have seen a comparable pattern during the COVID-19 pandemic.[14] EMS call volume has decreased, yet this reduction appears to be within the low-acuity patient population with 911 activations coming from sicker patients during the pandemic period.[15] Figure 1 shows that overall EMS calls have surged when new positive cases have surged, first in April then in July and again through much of the fall of 2020. By the first week of January, calls resulting in COVID-19 diagnosis had reached a towering third wave.
Figure 1: 911 Records with COVID-19 ED or Hospital Diagnoses
(Daily and 7-Day Moving Average, March 2, 2020 – February 15, 2021)
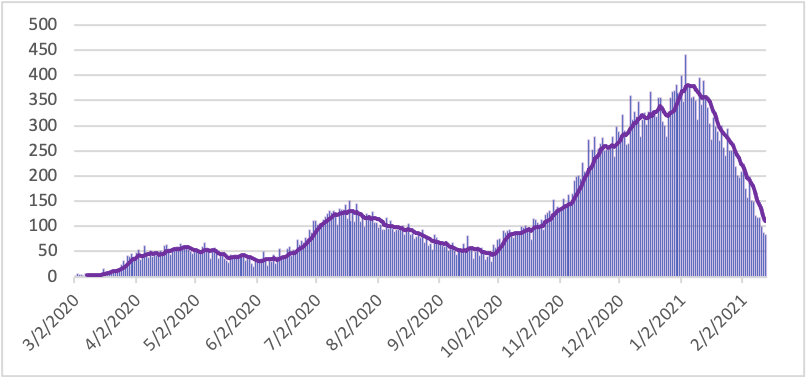
Chart by CSFE using data made available at ESO (2021).[16]
The current scope of practice model in use for EMTs and paramedics allows for the autonomous function that is necessary in the pre-hospital environment. This model is not, however, a highly flexible one. Thus, EMS providers are often unable to adjust their functionality quickly in times of crisis.[17] Researchers are now proposing an expanded scope of practice for EMS providers to raise adaptability and innovation by allowing them to function in expanded critical care environments and to supplement other allied health professionals in a myriad of practice settings. [18] In March 2020, the North Carolina Office of EMS (NCOEMS), which is responsible for credentialing and regulating emergency providers in the state, responded to pandemic needs by:
- Temporarily suspending General Statute 131E-158 which stipulates that an ambulance must be staffed by at least two EMS professionals. This suspension allows for one EMS provider to provide care while a non-EMS professional may drive the vehicle.[19]
- Temporarily suspending portions of North Carolina Administrative Codes 10A NCAC 13P .0501, .0502, .0504, and .0600. These suspensions directly relate to EMS education and credentialing requirements.[20]
- Providing guidance on alternative practice sites for EMS professionals.[21]
These provisions are designed to bolster the health care workforce and allow for flexibility during unexpected staff reductions. Educational requirements for EMS courses were adjusted to allow for high-fidelity simulation in lieu of on-site clinical rotations (as clinical sites increasingly forbade students from entering). Additionally, currently credentialed EMS professionals were given a six-month extension on their certification, delaying the need to complete continuing education requirements. While NCOEMS allows for alternative practice sites, these locations must comply with medical oversight requirements as set forth in General Statute 143-514 and the North Carolina Administrative Code 13P .0102.[22]
As we look beyond the immediate policy tweaks in response to the COVID-19 pandemic, there are opportunities for long-lasting impacts. A permanent adjustment of EMS educational regulations regarding clinical experiences could remove barriers related to clinical capacity for student interns. Temporary measures allow for up to 50% of an EMS student’s remaining clinical time to be substituted with high-fidelity simulation. A permanent regulation change would bring North Carolina EMS education in-line with the nursing profession. The North Carolina Board of Nursing clearly defines simulation pedagogy for nursing students and allows nursing programs to substitute high-fidelity simulation for clinical experience time under stipulations defined in 21 NCAC 36 .0321 (m), (n), and (o). Nationally accredited nursing programs are allowed to substitute up to 50% of clinical time in each course with simulation experiences.[23]
This provision was in-place prior to COVID-19 pandemic restrictions and allows for creative and substantive educational opportunities. Additionally, we must remain attentive to the needs of North Carolina EMS professionals and potential ways in which to sustain and promote innovation. One such innovative approach to meeting the needs of disparate communities is the Recognition of EMS Personnel Licensure Interstate Compact (REPLICA). The Compact allows EMS professionals to move across state boundaries with a legal privilege to practice extended from their “home state” into the “visiting state.” Currently, North Carolina and Florida are the only states in the southeastern region where this interstate licensure compact has not been adopted, thus limiting the ability for North Carolina to address short-term EMS worker shortages or crises. Furthermore, by restricting the movement of labor across North Carolina state lines, EMS professionals are bound to location unless they choose to navigate the burdensome reciprocity processes of neighboring states. The federal Interstate Commission for EMS Personnel Practice has drafted model legislative language that is freely available for REPLICA proposals at the state level.[24]
4. Bystanders as First Responders
Although the focus of this paper has been on EMTs and paramedics in their first-responder roles, the role of the general public should not be ignored. If spared from becoming a victim, members of the lay public are most commonly casual observers of an MCI. In the case of pandemic, however, the average person becomes an integral member of the first-response community. By simply engaging in public health measures such as facial coverings and social/physical distancing, our neighbors are fighting the virus alongside their medically-trained brethren.
Recommended public health precautions during the COVID-19 pandemic have become largely politicized[25], but their efficacy remains undeniable as a non-insignificant number of the general public have been unwilling to follow the recommended safeguards. Data show that cardiac arrests have increased during the pandemic with more arrests occurring at home.[26] In these circumstances, witness action is crucial as bystander CPR more than doubles one’s chances of survival.[27] Yet, the proportion of out-of-hospital cardiac arrest patients receiving bystander CPR has decreased significantly, as have overall survival rates.[28]
In order to increase bystander participation as de facto first responders, proper information about viral transmission and proper procedure is needed. Rescue breathing (i.e., mouth-to-mouth ventilation) during CPR has not been recommended for over a decade, instead bystander CPR should focus on a hands-only approach.[29] Additionally, aware that even hands-only bystander CPR may create aerosolized respiratory droplets, pandemic recommendations include a cloth covering for the victim’s face.[30]
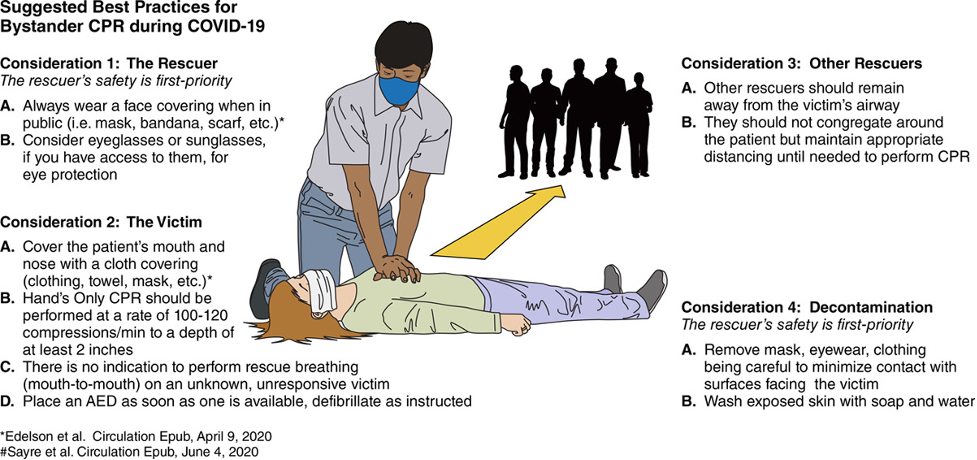
Image from Perman (2020)
The general public is now on the front-lines of the pandemic response. It has been shown that higher levels of social capital (shared group norms and values) directly affect disaster response efforts within the community[31] and encourage collective action towards a shared goal.[32] With a focus on community wellbeing and connection, recruitment into basic tenets of public health precautions may be more successful.
5. Policy Implications
A Presidential Policy Directive (PPD-8), issued by President Obama in March 2011, set a federal-level foundation for preparation and response to multiple national threats, including pandemic scenarios.[33] PPD-8 can be used by various state and local entities to aid in planning for large disruptive events. What PPD-8 clearly underscores is the importance of assessment and planning. Thus, EMS professionals not only have a duty-to-act but also a duty-to-plan.[34] Although planning and preparation are the first steps along the mortality/morbidity-reduction road, pre-pandemic study of emergency medicine physicians has shown that these medical professionals ranked the Strategic National Stockpile 36th out of forty core competencies within disaster medicine.[35] Other low-scoring areas were isolation/quarantine (20th), prehospital management (25th), and contingency planning (30th). The pre-pandemic minimization of these factors has borne a renewed concern over the fragility of the Strategic National Stockpile and its associated supply chains.[36] In response, FEMA was granted expanded authority to respond to the COVID-19 pandemic.[37]
The COVID-19 pandemic will undoubtedly shape local, state, and federal policy for years to come. Levels of preparedness and timeliness of action will be scrutinized, ultimately resulting in changes to NIMS and CDP training for EMS professionals. The catalyst of policy change in this case will result from a focusing event.[38] An extension of John Kingdon’s policy streams model, focusing events bring previously obscured issues to the forefront. These are events that are large in scale, occur suddenly, and are somewhat rare.[39] The COVID-19 pandemic will certainly serve as a focusing event, pushing policymakers and stakeholders towards changes in preparedness and public health policy.
6. Conclusion
The COVID-19 pandemic has strained the American health care system, and EMS has not been immune to that pressure. Pre-pandemic EMS training and disaster medicine focuses have proven to be insufficient for such a protracted and widespread event. While EMS professionals are highly trained in the management of emergency situations and MCI events, little has prepared them to quickly tackle a combatant as extensive, agile and evasive as the SARS-CoV-2 virus.
Past pandemic responses have provided a basic template for EMS professionals, but the COVID-19 pandemic will certainly push knowledge and capabilities forward. Deficiencies have been exposed and innovative solutions have risen to the surface. EMS professionals have proven themselves capable in the public health and disaster medicine realms. EMTs and paramedics have ranked among the most flexible of health care workers during the COVID-19 pandemic and continue to evolve their practice to serve the community.
Policy changes related to pandemic planning and response, both large and small, are on the horizon. As a focusing event, this pandemic will intensify concentration upon large-scale disease mitigation and preparedness. The health care spectrum will emerge stronger than ever with improved tools to combat future widespread events.
About the Author
Jackson D. Déziel is an Assistant Professor and Director of the Emergency Medical Care Program at Western Carolina University. Dr. Déziel began his health care career in 2000 in New Hampshire and has since worked as a paramedic in both urban and critical care settings. He earned a PhD in Public Policy from the University of North Carolina at Charlotte and his research interests embrace the intersection of EMS, health economics, and subsequent policy.

Further Readings
You are encouraged to delve further into the COVID-19 pandemic and its effects on the emergency health care system. Janet Bray, et al. (2020) discuss the consequences of the pandemic on bystander CPR.[1] The incidence of cardiac arrests occurring at home has increased significantly during the pandemic and it is recommended that you receive CPR training. For a wider view, the North Carolina Office of EMS has made publicly available their COVID-19 Response Documents and Links website.[2] Additionally, ESO has published a special COVID-19 edition of their EMS Index.[3] Each of these resources highlight and describe the EMS COVID-19 response on state and national levels. Lastly, you may explore John Kingdon’s Agendas, Alternatives, and Public Policies for a deeper discussion of the policy-making process as it pertains to major events.[4]
References
Allcott, Hunt, Levi Boxell, Jacob Conway, Matthew Gentzkow, Michael Thaler, and David Y. Yang. “Polarization and public health: Partisan differences in social distancing during the Coronavirus pandemic.” NBER Working Paper w26946 (2020).
Alwidyan, Mahmoud T., Joseph E. Trainor, and Richard A. Bissell. “Responding to natural disasters vs. disease outbreaks: Do emergency medical service providers have different views?.” International journal of disaster risk reduction44 (2020): 101440.
Birkland, Thomas A. “Focusing events, mobilization, and agenda setting.” Journal of public policy (1998): 53-74.
Birkland, Thomas A. ““The world changed today”: Agenda‐setting and policy change in the wake of the September 11 terrorist attacks.” Review of Policy Research 21, no. 2 (2004): 179-200.
Boehronger, Brad, Peter O’Meara, Gary Wingrove, and Nikiah G. Nudell. “An Emergency Amendment to the National Scope of Practice for Paramedics in the Setting of a Global Pandemic.” The Journal of Rural Health (2020).
Bray, Janet, Susie Cartledge, and Andrea Scapigliati. “Bystander CPR in the COVID-19 pandemic.” Resuscitation Plus (2020).
Catlett, Christina L., J. Lee Jenkins, and Michael G. Millin. “Role of emergency medical services in disaster response: resource document for the National Association of EMS Physicians position statement.” Prehospital emergency care15, no. 3 (2011): 420-425.
Chamlee-Wright, Emily, and Virgil Henry Storr. “Social capital as collective narratives and post-disaster community recovery.” The sociological review 59, no. 2 (2011): 266-282.
Chow‐In Ko, Patrick, Wen‐Jone Chen, Matthew Huei‐Ming Ma, Wen‐Chu Chiang, Chan‐Ping Su, Chien‐Hua Huang, Tsung‐Chien Lu, Fuh‐Yuan Shih, and Fang‐Yue Lin. “Emergency Medical Services Utilization during an Outbreak of Severe Acute Respiratory Syndrome (SARS) and the Incidence of SARS‐associated Coronavirus Infection among Emergency Medical Technicians.” Academic emergency medicine 11, no. 9 (2004): 903-911.
Coccolini, Federico, Massimo Sartelli, Yoram Kluger, Emmanouil Pikoulis, Evika Karamagioli, Ernest E. Moore, Walter L. Biffl et al. “COVID-19 the showdown for mass casualty preparedness and management: the Cassandra Syndrome.” World Journal of Emergency Surgery 15 (2020): 1-6.
ESO, “2020 ESO EMS Index: COVID-19 Special Edition.” accessed via https://298z52kdr59aqvzx2s3mgr16-wpengine.netdna-ssl.com/wp-content/uploads/2020/08/ESO-2020-COVID-Index.pdf (2020).
ESO, “COVID-19 Resource Center.” accessed via https://www.eso.com/covid-19/#section-ems-covid-19-and-influenza-like-illness-surveillance (2021)
Hick, John L., Dan Hanfling, Matthew K. Wynia, and Andrew T. Pavia. “Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2.” NAM Perspectives (2020).
Jensen, Jessica, and Steven Thompson. “The incident command system: a literature review.” Disasters 40, no. 1 (2016): 158-182.
Kahan, Jerome H. “Preparedness Revisited: W (h) ither PPD-8?.” Homeland Security Affairs 10, no. 2 (2014): 1-48.
Kingdon, John W.. Agendas, alternatives, and public policies. Vol. 45. Boston: Little, Brown (1984).
Kirsch, Thomas, Mark Keim, and Kandra Strauss-Riggs. “Characterizing the current state of training courses available to US disaster professionals.” Disaster medicine and public health preparedness 13, no. 5-6 (2019): 920-926.
Lerner, E. Brooke, Craig D. Newgard, and N. Clay Mann. “Effect of the Coronavirus Disease 2019 (COVID‐19) Pandemic on the US Emergency Medical Services System: A Preliminary Report.” Academic Emergency Medicine 27, no. 8 (2020): 693-699.
Lunn, Peter D., Cameron A. Belton, Ciarán Lavin, Féidhlim P. McGowan, Shane Timmons, and Deirdre A. Robertson. “Using Behavioral Science to help fight the Coronavirus.” Journal of Behavioral Public Administration 3, no. 1 (2020).
North Carolina Administrative Code 36 0.321, accessed via http://reports.oah.state.nc.us/ncac/title%2021%20-%20occupational%20licensing%20boards%20and%20commissions/chapter%2036%20-%20nursing/21%20ncac%2036%20.0321.html (2019).
North Carolina Office of EMS, “State Data Sheet.” accessed via https://continuum.emspic.org (2020a).
North Carolina Office of EMS, “High Consequences Pathogens.” accessed via https://ncems.org/latest/latest-sc2-respiratory-disease-uneditable.pdf (2020b).
North Carolina Office of EMS, “Temporary Suspension of GS 131E-158.” accessed via https://ncems.org/pdf/GSMemo-3-25-2020.pdf (2020c).
North Carolina Office of EMS, “Temporary Suspension of Portions of North Carolina Administrative Code.” accessed via https://ncems.org/pdf/EducationSuspensionCovid-19LetterFinal.pdf (2020d).
North Carolina Office of EMS, “Alternative Practice Settings.” accessed via https://ncems.org/pdf/AlternatePracticeSettingsPosition.pdf (2020e).
North Carolina Office of EMS, “COVID-19 Response Documents and Links.” accessed via https://ncems.org/covid-19-response.php (2020f).
Perman, Sarah M. “Overcoming fears to save lives: COVID-19 and the threat to bystander CPR in out-of-hospital cardiac arrest.” Circulation 142, no. 13 (2020): 1233-1235.
Petersen, Eskild, Marion Koopmans, Unyeong Go, Davidson H. Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, and Lone Simonsen. “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics.” The Lancet infectious diseases (2020).
Phillips, James P., Luca Ragazzoni, W. Greg Burel, Frederick M. Burkle, and Mark Keim. “Report from the COVID-19 Virtual Summit, Disaster Experts Speak Out, March 31, 2020.” Prehospital and disaster medicine 35, no. 4 (2020): 420-425.
REPLICA “Model Legislation” accessed via https://www.emscompact.gov/compact-information/replica-model-legislation/ (2018).
Sarin, Ritu R., Paul Biddinger, John Brown, Jonathan L. Burstein, Frederick M. Burkle, Douglas Char, Gregory Ciottone et al. “Core Disaster Medicine Education (CDME) for Emergency Medicine Residents in the United States.” Prehospital and disaster medicine 34, no. 5 (2019): 473-480.
Sasson, Comilla, Mary AM Rogers, Jason Dahl, and Arthur L. Kellermann. “Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis.” Circulation: Cardiovascular Quality and Outcomes 3, no. 1 (2010): 63-81.
Satty, Timothy, Sriram Ramgopal, Jonathan Elmer, Vincent N. Mosesso, and Christian Martin-Gill. “EMS responses and non-transports during the COVID-19 pandemic.” The American Journal of Emergency Medicine (2020).
Uy-Evanado, Audrey, Harpriya S. Chugh, Arayik Sargsyan, Kotoka Nakamura, Ronald Mariani, Katy Hadduck, Angelo Salvucci, Jonathan Jui, Sumeet S. Chugh, and Kyndaron Reinier. “Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic.” JACC: Clinical Electrophysiology (2020).
